Secondary Acute Myeloid Leukemia (sAML) is a subgroup of Acute Myeloid Leukemia (AML) associated with poor outcomes despite recent advancements in chemotherapy. CPX-351 (United States: Vyxeos®), a 1:5 liposomal encapsulation of daunorubicin and cytarabine was approved in 2017 by the US Food and Drug Administration (FDA) for the treatment of newly diagnosed Secondary AML. Previously, the conventional 7+3 Regimen (7 days of cytarabine and 3 days of daunorubicin) was considered first line for the treatment of sAML. However, the pivotal study that led to approval of CPX-351 demonstrated increased Overall Survival (OS) with CPX-351. We report a systematic review of published literature on the efficacy and safety of CPX-351 in patients with sAML, including data from post-market real-world experiences of patients.
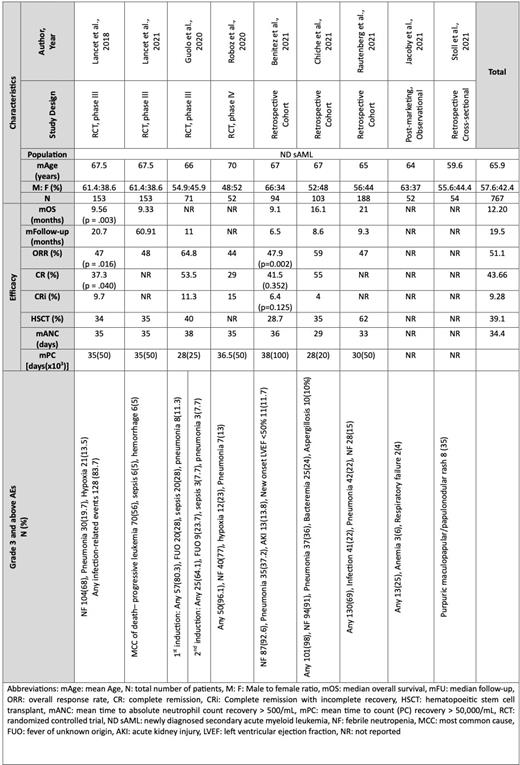
Materials and Methods Following PRISMA guidelines, we performed a comprehensive literature search for articles published after 2017 using PubMed, Embase, Clinical Trials.gov, Cochrane Library, and Web of Science. Initially 63 articles were identified, and after a thorough screening, we finalized 9 studies including 767 patients, illustrated in Table 1. We analyzed data from patients who received CPX-351 chemotherapy as first-line therapy for sAML. MeSH terms and keywords were 'CPX-351' and 'Leukemia, Myeloid, and Acute'.
Results The median age of patients was 65.9 years. Patients could receive up to two cycles of induction, and those who achieved complete remission (CR) or complete remission with incomplete recovery (CRi) could receive up to 2 cycles of consolidation with CPX-351. CPX-351 treatment showed median overall survival (mOS) of 12.20 months, CR rate of 43.66%, and an overall remission rate (ORR) of 51.1%. Hematopoietic Stem Cell Transplantation (HSCT) was performed in 39.1% patients. The mean time to absolute neutrophil count >500/mL (mANC) and platelet count >50,000/mL (mPC) recovery in patients who achieved OR was 34.4 days and 32.9 days, respectively. The most frequently reported greater than grade 2 adverse events (AEs) were febrile neutropenia (NF), opportunistic infections including pneumonia, and hypoxia.
Conclusion In sAML patients, the CPX-351 regimen is more effective and well tolerated as compared to the conventional 7+3 Regimen. The real-world data also points to CPX-351 as an efficient therapeutic agent for sAML patients facilitating HSCT in many patients with promising outcomes after transplantation. CPX-351 is a treatment of choice for patients aged >60 years. Future randomized prospective trials with longer follow-up periods are needed to consolidate these findings, and help us better understand the efficacy and survival outcomes of CPX351 regimens for sAML treatment.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal